Inflammatory Choroidal Neovascular Membrane
Dr. Shashank Somani, Dr. Sarang Lambat, Dr. Prabhat Nangia, Dr. Vinay Nangia
Suraj Eye Institute, 559 New Colony, Nagpur
Case Description
A male, 63 years of age, presented to us with the complaint of seeing a black spot in front of the right eye since few days. He was a known case of diabetes mellitus under treatment since 6 years. On examination his best corrected visual acuity was 6/12(p), N8 in right eye and 6/9, N6 in left eye. Anterior segment examination was normal. Intraocular pressure recorded by Goldmann applanation tonometer was 14 mmHg in both eyes.

Figure 2: Fundus photograph of the left eye shows multiple healed choroiditis lesions in the left eye. (green arrows)
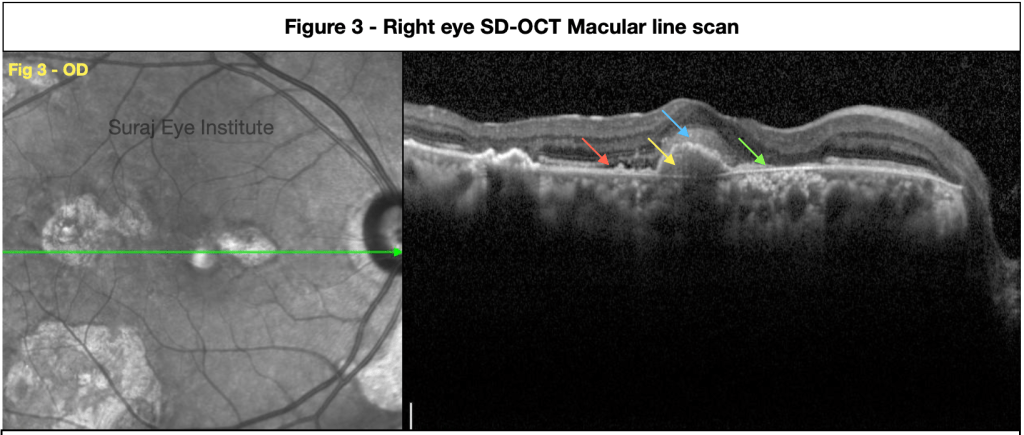
The area nasal to the CNV shows loss of photoreceptors and RPE with intermittent RPE clumping along with hyperreflectivity of the choroid with evident shrinking of the choroidal vasculature suggestive of a chorio-retinal scar (Green arrow).




Discussion
Our patient presented with recent visual loss in the right eye and on the basis of characteristic findings on multimodal imaging (MMI) we were able to conclude that he had an inflammatory CNV (iCNV). The patient was advised to undergo injection anti VEGF. Ocular inflammation though not common cause for CNVM formation, but it is just next to AMD and Myopia. This patient did not have any evidence of age related macular degeneration and he was not myopic. Diagnosis of an Inflammatory CNV is difficult especially when it is associated with areas of active or healed choroiditis. It is important to investigate such patients in detail to determine whether we are dealing with an active inflammation or an iCNV. MMI guides us to accurately distinguish between the two.
The development of iCNV is associated with infective and non infective causes of posterior uveitis. The infective causes include histoplasmosis, toxoplasmosis, toxocariasis, tuberculosis, congenital rubella, and West Nile virus. The non infective causes include punctate inner choroidopathy, multifocal choroiditis, serpiginous choroiditis and Vogt-Koyanagi-Harada (VKH) disease. It has been thought that i-CNV can occur either directly from an angiogenic stimulus mediated by local inflammation or it can result from a degenerative disruption in the Bruch’s membrane–RPE complex, or both. Majority of i-CNVs are type 2 lesions with abnormal growth of vasculature into the outer retinal space. CNV lesion may be missed initially due to the presence of associated features such as inflammatory lesions, scars, and pigmentation, as well as intra- or subretinal fluid accumulation. It is imperative to evaluate such patients in detail and do MMI to ensure that typical findings in each imaging modality are available for accurate diagnosis. On SDOCT the retinal features of choroiditis lesions may be similar to the iCNV. Finger like projections from the iCNV in the outer retina labelled as the ‘pitchfork sign’ helps us to differentiate iCNV from ocular inflammation. Findings on each imaging modality needs to be interpreted with caution.
Anti VEGF agents are very effective in iCNV. Intravitreal dexamethasone implant, methotrexate, or triamcinolone acetonide can also be considered, which help to reduce the size of the CNV lesion.
ReadWise
- Agarwal A, Invernizzi A, Singh RB, Foulsham W, Aggarwal K, Handa S, Agrawal R, Pavesio C, Gupta V. An update on inflammatory choroidal neovascularization: epidemiology, multimodal imaging, and management. J Ophthalmic Inflamm Infect. 2018 Sep 12;8(1):13. doi: 10.1186/s12348-018-0155-6.
- Neri P, Lettieri M, Fortuna C, Manoni M, Giovannini A. Inflammatory choroidal neovascularization. Middle East Afr J Ophthalmol. 2009 Oct;16(4):245-51. doi: 10.4103/0974-9233.58422.
Dr. Sarang Lambat
MS, FRF
Consultant
Vitreoretinal services
Suraj Eye Institute
Nagpur
Email – education@surajeye.org
